Fabric selection plays a critical role in ensuring patient and healthcare worker safety. The specific properties of hospital gowns fabric directly influence infection control and patient comfort within medical environments. Suboptimal fabric choices can increase the risk of pressure injuries and restrict patient mobility. Patients also often lack control over gown designs, which impacts comfort and personal dignity.
Key Takeaways
- Different hospital gown fabrics offer various levels of protection and comfort. Non-woven fabrics like SMS provide strong barriers against germs, while woven fabrics like cotton offer comfort.
- Hospital gowns are tested for how well they stop liquids and germs. The AAMI levels (1-4) show how much protection a gown gives, with Level 4 being the highest.
- Reusable hospital gowns are better for the environment and can save money. They reduce waste and use less energy and water compared to disposable gowns.
Understanding Hospital Gowns Fabric Categories

Non-Woven Fabrics for Hospital Gowns
Non-woven fabrics are a common choice for hospital gowns. Manufacturers create these materials by bonding fibers together rather than weaving them. One key method is spunbonding. This process uses heat and pressure to create a strong, lightweight fabric. Another important technique is meltblowing. Here, molten material extrudes onto the fabric, then cools and solidifies. This layer provides an effective barrier against liquids and bacteria. Combining spunbond and meltblown processes results in a fabric that is lightweight, breathable, and resistant to tearing. This combination effectively prevents infection spread.
Woven Fabrics for Hospital Gowns
Woven fabrics offer another option for hospital gowns, particularly for reusable types. Typical fiber compositions include 100% monofilament polyester. Some woven fabrics incorporate 99% polyester with a 1% carbon fiber stripe. This carbon fiber helps with static dissipation and fluid resistance. Historically, cotton and poly-cotton blends were common for reusable gowns. However, their porous properties allow microorganisms to pass through. Micro-filament fabrics feature tightly woven, very fine filaments. Manufacturers reprocess these with a hydrophobic agent to enhance their protective qualities.
Composite Materials in Hospital Gowns
For certain medical procedures, a single-ply material may not offer sufficient barrier properties. In these cases, composite materials provide enhanced protection. Manufacturers create composites by incorporating additional layers, coatings, or reinforcements. This layering improves product attributes like absorbency, slip resistance, and strength. A common material combination involves wood pulp and polypropylene (PP) fibers. For instance, a blend of 70% wood pulp with 30% PP fibers creates a single-layer spunlace fabric. Wood pulp rapidly absorbs liquids, while PP fibers provide a durable structure. This composite allows air circulation while blocking bacteria and fluids. Composite fabrics can also include inorganic antibacterial agents, such as silver ion-modified fibers, integrated during fiber extrusion.
Properties of Common Hospital Gowns Fabric Types

Understanding the specific properties of different hospital gowns fabric types helps healthcare facilities make informed choices. Each material offers unique advantages for various medical settings and levels of protection.
Polypropylene Spunbond Fabric
Polypropylene spunbond fabric is a popular choice for disposable hospital gowns. Manufacturers create this material by extruding molten polypropylene and then spinning it into fine fibers. They then bond these fibers together using heat and pressure. This process results in a lightweight, breathable, and cost-effective fabric. It offers a basic level of fluid resistance and particulate barrier. Healthcare workers often use polypropylene spunbond gowns for low-risk procedures or general patient care where extensive barrier protection is not the primary concern.
Spunbond Meltblown Spunbond (SMS) Fabric
SMS fabric represents a significant advancement in non-woven technology for hospital gowns. It consists of three layers: two outer spunbond (S) layers and an inner meltblown (M) layer. The spunbond layers provide strength and durability, while the meltblown layer acts as a critical barrier. This meltblown layer effectively blocks liquids and microscopic particles.
SMS nonwovens demonstrate superior efficiency in preventing the transmission of S. aureus and E. coli in saline solutions compared to woven fabrics. Polypropylene-based gowns, including SMS laminates, provide the greatest protection against microbial penetration among various materials tested. The meltblown layer in SMS fabric provides a barrier impervious to pathogens and achieves >95% viral filtration efficiency (VFE) for viruses as small as 0.1 microns.
SMS fabric offers excellent fluid resistance. Consider the following comparison of hydrostatic pressure, which measures a fabric’s resistance to water penetration:
| Material | Weight (gsm) | Hydrostatic Pressure (cm H2O) |
|---|---|---|
| Spunbond Polypropylene | 17 | 3.0 |
| SMS | 17 | 19.2 |
| Spunbond Polypropylene | 40 | 12.4 |
| SMS | 36 | 79.4 |
This data shows SMS fabric significantly outperforms spunbond polypropylene in fluid resistance, especially at higher weights. SMS also excels in bacterial filtration efficiency (BFE):
| Material | BFE (%) |
|---|---|
| SMS | >99.9% |
| Polypropylene (PP) | 90–98% |
| Polyethylene (PE) | 85–95% |
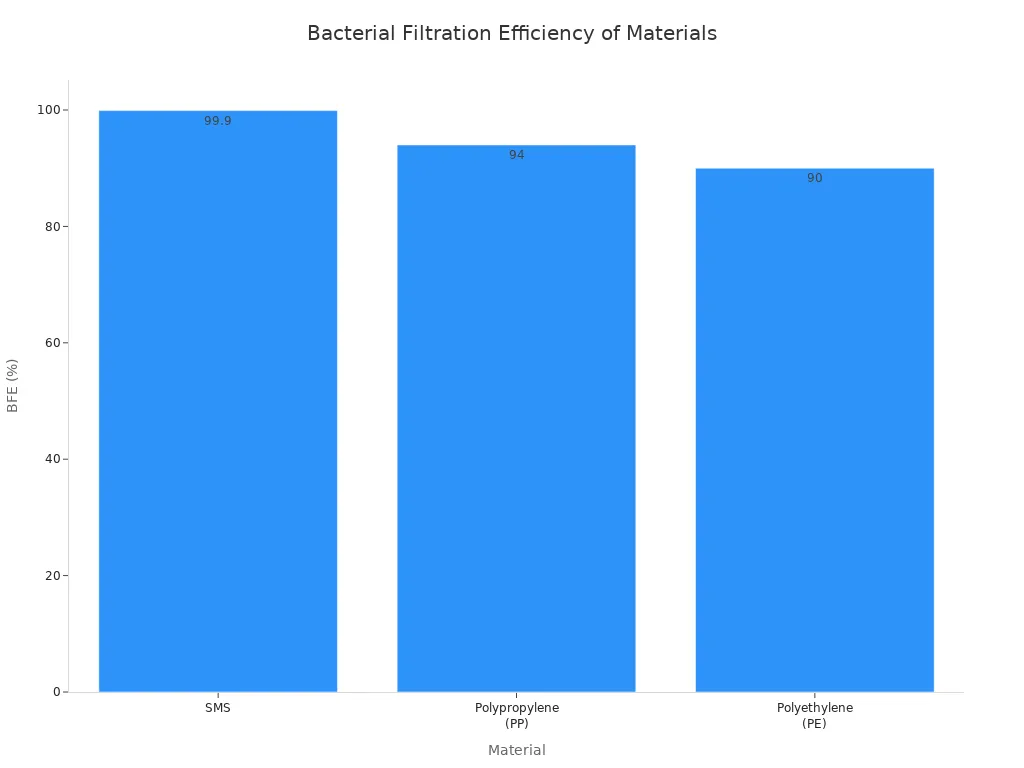
SMS gowns significantly reduce contamination risk and bacterial transmission. Studies show SMS gowns reduced contamination risk by 68% compared to standard PP gowns. They also reduced bacterial transmission rates by 67% compared to woven textiles. This makes SMS a preferred material for surgical gowns and other high-barrier applications.
Polyethylene Fabric
Polyethylene (PE) fabric is known for its exceptional impermeability. Manufacturers often use it for isolation gowns where a complete liquid barrier is essential. Chlorinated polyethylene (CPE) gowns, a common type, offer robust protection.
- CPE’s chemical structure provides strength and flexibility. This makes it suitable for disposable protective apparel in both wet and dry conditions.
- CPE gowns are waterproof. Special polymer cement and adhesive paste form a strong waterproof layer.
- They exhibit aging resistance, allowing use in severe weather and harsh environments. They also have sufficient resistance to ozone, which is crucial during pandemics.
- Doctors wear CPE isolation gowns during operations to maintain an aseptic state and ensure patient safety.
- CPE gowns help prevent the spread of bacteria and viruses in hospitals and nursing units, ensuring hygiene.
Ritmed® AssureWear® Polyethylene Isolation Gowns, for example, feature an over-the-head design with thumb loop cuffs. These gowns are made from spunbond polyethylene and have sewn seams for superior strength. They are latex-free and classified as an isolation gown application type. Their impervious nature indicates their barrier effectiveness.
Cotton and Cotton Blend Hospital Gowns Fabric
Cotton and cotton blend fabrics are traditional choices for reusable hospital gowns. They offer significant comfort and breathability for patients.
Crafted from comfortable and breathable materials like cotton or cotton blends, our patient gowns prioritize patient comfort while ensuring proper coverage.
While comfortable, cotton’s porous nature means it offers minimal fluid resistance. This limits its use in environments requiring high barrier protection. Cotton blends, often with polyester, aim to improve durability and reduce shrinkage while retaining some of cotton’s comfort. Maintaining the integrity of these gowns requires specific laundering protocols. Soiled gowns undergo a comprehensive cleaning process. This may include washing, disinfection, and sterilization. The specific steps depend on the type of gown and the level of contamination it has experienced. Reusable isolation gowns, such as yellow medium-weight broadcloth gowns, are constructed from a durable and breathable 55/45 polyester-cotton blend fabric. This blend is designed to endure multiple uses and washes without compromising its protective qualities. This makes it suitable for demanding healthcare environments.
Polyester and Polyester Blend Hospital Gowns Fabric
Polyester and polyester blend fabrics are common in reusable hospital gowns due to their durability, strength, and resistance to shrinking and wrinkling. Polyester offers good chemical resistance and does not absorb liquids, making it a better barrier against certain contaminants than cotton.
| Feature | Polyester Fabric | Cotton Fabric |
|---|---|---|
| Chemical Resistance | Good barrier to acids and biological contaminants | Susceptible to acid spills; minimal fluid resistance |
| Liquid Absorption | Does not absorb liquids | Not fluid resistant, especially to acids |
| Suitability | Biomedical research, blood testing labs | Requires additional protection for corrosive materials |
| Cost | Less expensive to manufacture | Often more expensive (for 100% cotton) |
Polyester lab coats, for instance, are durable and long-lasting. Cotton lab coats, however, offer minimal resistance to fluids and chemicals. Polyester blends often combine polyester with cotton to balance comfort with enhanced durability and fluid resistance. These fabrics can withstand numerous wash cycles while maintaining their protective qualities.
| Fabric | Cycles to 50% Strength | Cycles to Visible Wear | Tensile Strength Retention (after 200 cycles) |
|---|---|---|---|
| High-tenacity Polyester | 250 | 300 | >85% |
| 80/20 Blend | 150 | 200 | N/A |
| 100% Polyester | N/A | N/A | >92% (after 100 autoclave cycles) |
A dialysis center’s facility manager reported that gowns failing below 90% of their original tensile strength after 20 washes were deemed unfit. This prompted a shift to blended polyester, which maintained 95% strength after 60 washes. This demonstrates the superior longevity and cost-effectiveness of polyester and its blends in reusable hospital gowns.
Key Performance Criteria for Hospital Gowns Fabric
Healthcare facilities carefully evaluate several key performance criteria when selecting hospital gowns fabric. These criteria ensure patient safety, healthcare worker protection, and operational efficiency.
Fluid Resistance and Barrier Protection
Fluid resistance is a primary concern for hospital gowns. It prevents the penetration of blood, bodily fluids, and other liquids. The Association for the Advancement of Medical Instrumentation (AAMI) established a classification system (Levels 1-4) to assess the fluid permeability of disposable gowns.
- Level 1 gowns offer minimal barrier protection against low fluid exposure. Manufacturers test these gowns for water spray impact only, using methods like AATCC 42.
- Level 2 gowns provide light to moderate protection against fluid penetration. They undergo testing for both water spray impact (e.g., AATCC 42) and hydrostatic pressure (e.g., AATCC 127).
- Surgical gowns, often Level 3 and Level 4, use AAMI designations. They feature reinforced barrier protection in critical zones for critical procedures.
AAMI levels for hospital gowns fabric are determined using standardized testing methods. ASTM F1670 and ASTM F1671 are the most stringent. These tests involve bodily fluid and blood-borne pathogen simulants. Only gowns passing ASTM F1671 are classified as Level 4. This indicates impermeability to viral penetration. Lower levels (1, 2, and 3) are tested against water. They show increasing resistance to liquids with higher surface tension. Manufacturers also report performance against AATCC 42 and AATCC 127. European standards use ISO for similar barrier performance evaluation.
Regulatory requirements differ for surgical and isolation gowns.
- Surgical Gowns:
- The critical zone comprises at least the front panel (area A) and lower sleeves (area B).
- Classification is based on the lower performing component of these two areas.
- The entire front of the gown (areas A, B, and C) must have a barrier performance of at least Level 1.
- The back of the gown (area D) can be non-protective.
- Isolation Gowns:
- The whole garment is considered a critical zone. This is due to unpredictable potential contact with blood, body fluids, and other potentially infectious materials (OPIM).
- The entire isolation gown, including seams (excluding cuffs, hems, and bindings), must achieve claimed barrier performance.
- Open-backed isolation gowns do not meet critical area parameters. They cannot receive a rating.
The FDA considers surgical gowns as Class II devices. They require a pre-market notification (510k submission). Surgical gowns must be labeled as AAMI Level 3 or 4 if marketed as ‘surgical’ in the US. They cannot claim to be AAMI Level 1 or 2 if marketed as ‘surgical’. Isolation gowns can be rated AAMI Level 1-4 or non-rated. Levels 1 & 2 isolation gowns are Class I devices. They do not require pre-market notification. Levels 3 & 4 isolation gowns are high-risk devices. They require pre-market notification. Both gown types fall under 21 CFR 878.4040. The FDA considers gowns with moderate to high barrier protection (Levels 3 & 4) as higher-risk devices.
The following table summarizes the AAMI levels and their corresponding test methods and barrier effectiveness:
| Level | Test | Liquid Challenge | Result | Expected Barrier Effectiveness |
|---|---|---|---|---|
| 1 | AATCC 42 Impact Penetration | Water | ≤ 4.5 g | Minimal water resistance (some resistance to water spray) |
| 2 | AATCC 42 Impact Penetration | Water | ≤ 1.0 g | Low water resistance (resistant to water spray and some resistance to water penetration under constant contact with increasing pressure) |
| AATCC 127 Hydrostatic Pressure | Water | ≥ 20 cm | ||
| 3 | AATCC 42 Impact Penetration | Water | ≤ 1.0 g | Moderate water resistance (resistant to water spray and some resistance to water penetration under constant contact with increasing pressure) |
| AATCC 127 Hydrostatic Pressure | Water | ≥ 50 cm | ||
| 4 | ASTM F1670 Synthetic Blood Penetration Test (for surgical drapes) | Surrogate Blood | no penetration at 2 psi (13.8 kPa) | Blood and viral penetration resistance (2 psi) |
| ASTM F1671 Viral Penetration Test (for surgical and isolation gowns) | Bacteriophage Phi-X174 | no penetration at 2 psi (13.8 kPa) |
Microbial Barrier Effectiveness
Microbial barrier effectiveness measures a fabric’s ability to block bacteria and viruses. This is crucial for infection control. For products designed to block airborne particulates and biological contaminants, filtration efficiency is the most essential testing category. This family of tests provides quantifiable data on the material’s ability to act as a physical barrier against microorganisms and aerosols.
The following table outlines common test methods for microbial barrier effectiveness:
| Test Type | Target Material | Standard Protocol (Example) | Key Performance Measure |
|---|---|---|---|
| Bacterial Filtration Efficiency (BFE) | Surgical Masks, Gowns | ASTM F2101 | Measures percentage of Staphylococcus aureus (average size 3.0 μm) filtered by the material. |
| Viral Filtration Efficiency (VFE) | Respirators, Face Masks | ASTM F2101 Modified | Measures percentage of bacteriophage ΦX−174 (average size 0.027 μm) filtered. |
| Particle Filtration Efficiency (PFE) | Cleanroom Filters, Media | ASTM F2299 | Measures the efficiency of the material against non-viable particle sizes (e.g., 0.1 to 5.0 μm). |
| Differential Pressure (ΔP) | All Barrier Textiles | MIL-M-36954C | Measures air permeability (breathability), ensuring filtration does not compromise user comfort or safety. |
The viral filtration efficiency (VFE) test is particularly crucial. Viruses are significantly smaller than bacteria. This makes them the ultimate challenge for fine filter media. A high VFE rating is non-negotiable for any product claiming protection against airborne viral pathogens. Labs must also ensure the material’s air permeability (measured via ΔP) remains low enough for user safety. This provides a critical balance between breathability and protection.
For bacterial filtration, fabrics must achieve a minimum Bacterial Filtration Efficiency (BFE) of 98%. ASTM F2101 measures this. For antimicrobial activity, fabrics need to demonstrate a reduction of at least 3 log in microbial activity. This signifies killing 99.9% of targeted pathogens. ISO 20743 evaluates this.
Breathability and Comfort
Breathability in fabrics, including those used for hospital gowns, is measured by their air permeability rating. This indicates how easily air passes through the material. This rating is crucial for specific applications. High ratings signify more breathable fabrics. Low ratings indicate less breathability. Several factors influence a fabric’s air permeability. These include fiber thickness (thinner fibers generally increase permeability), weave type (tighter weaves decrease airflow, while looser weaves enhance it), and fabric finish (some finishes block air passage, while others enhance breathability). Common testing methods for air permeability include ASTM D737 and ISO 9237. These involve specialized equipment to measure the rate of airflow through fabric samples. The results determine the air permeability rating. This guides material selection for optimal performance.
For general fabrics, air permeability typically ranges from 100 to 300 L/m²/s. Fabrics with low air permeability, often under 100 L/m²/s, are less breathable. Manufacturers use them in protective clothing where restricted airflow is desired. High air permeability, exceeding 300 L/m²/s, indicates very breathable fabrics. These are suitable for sportswear and activewear. Medical textiles, such as those for hospital gowns, have unique requirements for ‘controlled permeability’. This balances protection and breathability. It ensures proper air exchange for patient comfort and safety.
Traditionally, reusable surgical gowns were made from cotton muslin. This was a loosely woven, highly breathable fabric with high air permeability. However, its low liquid-penetration resistance led to its decline in use. Modern gowns often use polyester or polyester-cotton blends. While polyester-cotton blends offered good thermal comfort, they also faced challenges with liquid penetration protection. Tightly woven filament polyester fabrics offer increased protection. However, they can cause discomfort due to reduced thermal comfort. Nonwoven fabrics, commonly used for single-use gowns, include spunlace, spunbond–meltblown–spunbond (SMS), and wet-laid materials. Some nonwoven gown fabrics were evaluated as cooler due to lighter weight. However, conventional nonwoven fabrics have been challenged for their low air permeability and moisture vapor transmission rate. This impacts comfort levels.
Several fabric properties contribute significantly to patient thermal comfort and moisture management:
- Good moisture properties, fast drying, and low thermal and evaporative resistance contribute to higher comfort. Polyester fabric 8 for sportswear is an example.
- High thermal and vapor resistance and long drying times lead to less comfort. Fabric 4 is an example.
- Good moisture management properties, low thermal and vapor resistance, and short drying times characterize comfortable fabrics. Fabric 10 is an example.
- Higher thermal and vapor resistance, lower vapor permeability, and longer drying times are associated with less comfortable fabrics. Heat protection fabrics 18, 5, 4, 10, 2, 9, and 17 are examples.
Fabric mass and thickness influence thermal and water vapor resistance. Reducing them lowers vapor resistance. This is beneficial in hot conditions. Liquid moisture transfer properties are critical in hot conditions with high sweating rates. Fabrics that quickly absorb and transport moisture away from the skin enhance comfort. Wet knitwear significantly reduces comfort. Increased moisture in the skin-clothing microclimate decreases perceived comfort. A strong relationship exists between increased wetness perception and reduced thermal comfort. In warm ambient conditions, skin wetness relates more strongly to perceived thermal comfort than skin surface temperature.
Significantly positive correlations exist between drying time, evaporative resistance (Ret), and thermal resistance (Rct). This indicates that fabrics with greater thermal and moisture resistance take longer to dry. Drying time negatively correlates with moisture spreading speed (MWRB) and moisture radius on the external face (SSB). This means faster moisture spreading and higher moisture radius contribute to faster drying. The thermo-physiological comfort performance (TCP) model includes key fabric parameters. These include mass, moisture spreading speed, and evaporative resistance. Fabric 8 (86% PES + 14% EL) was identified as the most comfortable. This was due to its good thermoregulatory properties. Wear trials confirmed this, where over 80% of participants found it most comfortable.
Durability and Reusability
Durability is a crucial factor for reusable hospital gowns. It determines how many times a gown can withstand laundering and sterilization cycles while maintaining its protective properties.
The median lifespan of a reusable isolation gown is approximately 64 washes. These reusable gowns are typically made from woven polyester fabric.
This longevity makes reusable gowns a sustainable option. However, facilities must implement strict quality control measures. These ensure gowns retain their barrier integrity after each wash. Regular inspection for tears, holes, or compromised seams is essential.
Cost-Effectiveness and Environmental Impact
Healthcare facilities increasingly consider both cost-effectiveness and environmental impact when choosing hospital gowns.
A life cycle assessment comparing reusable and disposable gown systems at the healthcare facility level revealed significant environmental benefits for reusable gowns:
- 28% reduction in energy consumption
- 30% reduction in greenhouse gas emissions
- 41% reduction in blue water consumption
- 93% reduction in solid waste generation
The US healthcare sector contributes significantly to waste and greenhouse gas emissions. The perioperative service alone generates up to 70% of solid waste in US hospitals. This amounts to 2.8 billion pounds annually. Operations typically produce about 50 pounds of waste per case. Orthopedic and cardiac operations generate up to 200 pounds. Waste production in US hospitals has increased by 15% annually since 1992. This is largely due to the increased use of disposable equipment. Disposable textiles, including surgical gowns, are a major contributor to operating room waste.
The following table compares the environmental impact of reusable versus disposable surgical gowns:
| Environmental Impact | Reusable Surgical Gowns | Disposable Surgical Gowns |
|---|---|---|
| Energy Consumption | 4–15 MJ | 16–35 MJ |
| Water Usage | 2.9 gallons | 3.7 gallons |
| Carbon Footprint | 2–3 times smaller | Larger |
| Natural Resource Energy Consumption Reduction | 64% | N/A |
| Greenhouse Gas Emissions Reduction | 66% | N/A |
| Blue Water Conservation Reduction | 83% | N/A |
| Solid Waste Generation Reduction | 84% | N/A |
Research consistently shows that reusable healthcare textiles (HCTs), including surgical gowns, lead to reduced environmental impacts compared to their disposable counterparts. These benefits include lower carbon emissions, decreased water usage, less solid waste, and reduced energy consumption. The COVID-19 pandemic further highlighted the stability of circular reusable PPE systems over linear disposable supply chains. Despite these environmental advantages, reusable HCTs currently represent a small fraction of the U.S. PPE supply.
The environmental footprint of both reusable and disposable PPE can be reduced through localized manufacturing. This minimizes shipping distances. While reusable gowns are heavier, the environmental impact of their transportation is relatively small compared to manufacturing processes. Transporting Category A waste (highly infectious material) is significantly more expensive and complex than regulated medical waste. It requires more packaging and potentially complicated routes. Disposable PPE can add 60–70 pounds of packaging material per bin. This increases transportation costs and environmental effects. Incorrect triaging of items in hospitals leads to up to 70% of regulated medical waste being misclassified. This further burdens economic and environmental costs. Reducing PPE recommendations based on scientific understanding of risk, as seen with MRSA and VRE, can also benefit the environment.
A comparison of lifecycle costs also favors reusable options:
| Factor | Disposable Gowns (Before Conversion) | Reusable Gowns (After Conversion) | Savings/Reduction | | :———————————– | :——————————– | :—————- | | Total Waste Volume (lbs per APD) | 19 | 17.4 | 1.7 lbs (9%) | | EVS Expense (cents per APD) | $2.06 | $1.88 | 18¢ (9%) | | Total Waste & Labor Savings (per APD) | N/A | N/A | 30¢ | | Cost per Gown Use (including laundering)| N/A | 58¢ (13¢ gown + 45¢ laundering) | N/A | | Single Use Gown Cost | 60¢ | N/A | N/A | | Net Cost per Gown (after waste savings) | N/A | 28¢ | 53% savings | | UCLA Health Annual Savings | N/A | $450,000 | N/A | | UCLA Health Waste Diverted | N/A | 1,180 tons | N/A | | Carilion Clinic Cost per Gown Use | 79¢ | 39¢ | 50% savings | | Carilion Clinic Savings (3 years) | N/A | $850,000 | N/A | | Carilion Clinic Waste Eliminated (3 years)| N/A | 515,000 lbs | N/A | | Surgical Instrument Recovery (per procedure)| N/A | $1.50 | N/A | | UNC Rex Healthcare Annual Instrument Savings| N/A | $60,000 | N/A | | Cleanroom Coveralls Cost Savings | N/A | 58% | N/A |
These figures demonstrate that converting to reusable gowns can lead to substantial financial savings and waste reduction for healthcare systems.
Informed selection of hospital gowns fabric remains paramount for optimal patient care and safety. Ongoing advancements, such as AGXX technology, significantly enhance infection control by effectively killing bacteria and viruses. Future innovations also focus on sustainable materials like Polylactic Acid (PLA), which reduces environmental impact. These developments promise safer, more eco-friendly medical textiles.
FAQ
What is the main difference between woven and non-woven hospital gown fabrics?
Woven fabrics interlace threads, offering durability for reusable gowns. Non-woven fabrics bond fibers together, providing lightweight, disposable options with effective barrier properties.
Why do hospitals use SMS fabric for many gowns?
SMS fabric offers superior fluid resistance and microbial barrier effectiveness. Its multi-layered structure blocks liquids and pathogens, significantly reducing contamination risks during medical procedures.
Are reusable hospital gowns more environmentally friendly than disposable ones?
Yes, studies show reusable gowns significantly reduce environmental impact. They consume less energy and water, produce fewer greenhouse gas emissions, and generate substantially less solid waste over their lifecycle. ♻️
Post time: Jan-29-2026
